Within our guts is a tiny ecosystem populated by trillions of microorganisms. These germs have an effect on digestion, the immune system, and even mind functioning. Scientists have additionally began investigating the potential function of intestine micro organism in psychiatric and neurological situations, together with neurodegenerative illnesses like Alzheimer’s and Parkinson’s. If intestine microbes show influential, this might reveal how these illnesses work, resulting in earlier detection and new remedy targets.
Neurodegenerative illnesses progressively injury and kill nerve cells, inflicting issues with psychological or motion perform, and generally each. Over the previous 30 years, these illnesses have grown more common with the world’s more and more older inhabitants, but there are not any cures and few efficient therapies. Alzheimer’s and Parkinson’s illnesses prepared the ground, affecting hundreds of thousands of individuals worldwide.
These illnesses come up from combos of genetic, environmental, age-related, and way of life elements, however usually, medical doctors can’t pinpoint a trigger. Given that the mind connects with the intestine, scientists are more and more wanting on the potential function of intestine microbes.
Much of this analysis has centered on Parkinson’s, which is related to gastrointestinal points. But preliminary connections between the intestine microbiome and different neurodegenerative illnesses, like Alzheimer’s and amyotrophic lateral sclerosis (ALS), are additionally rising.
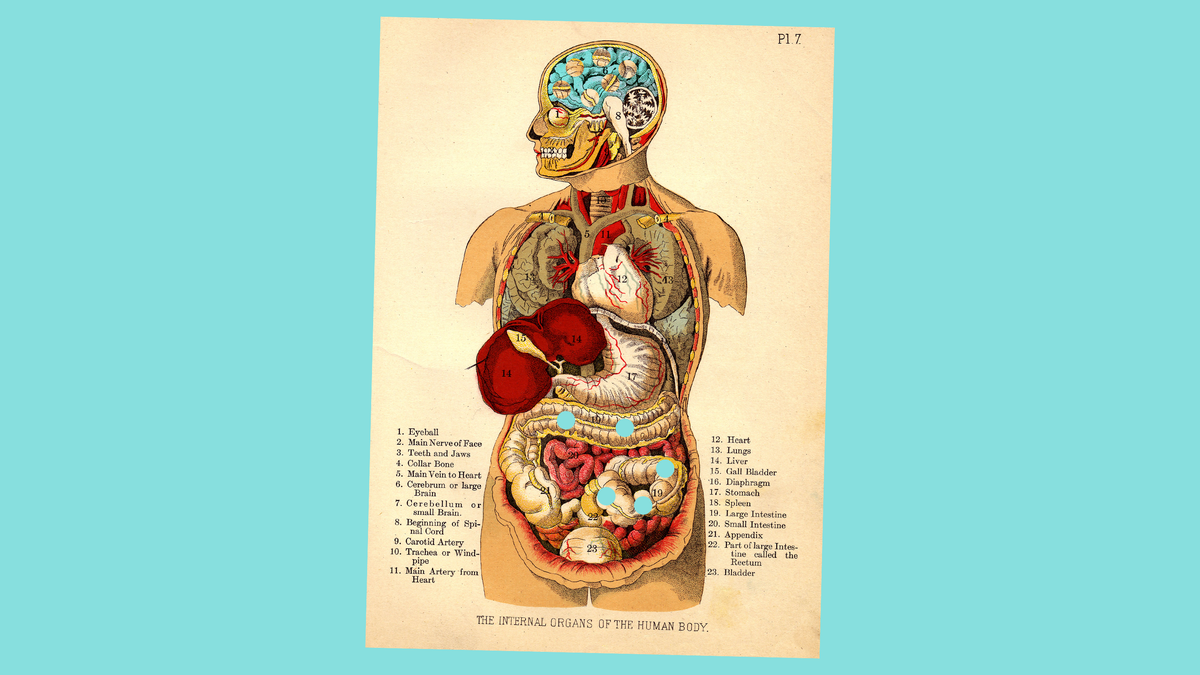
Bacteria account for almost all of the microorganisms in our guts, they usually’re in direct and oblique communication with the nervous system, which controls psychological capabilities, motion, sensory notion, and automated processes like respiration.
G/O Media could get a fee
Through a two-way connection known as the gut-brain axis, our microbes could possibly be liaising with the mind by way of nerves and chemical pathways. For instance, intestine micro organism can synthesize neurotransmitters, the mind’s molecular messengers, and different chemical compounds used within the mind. When absorbed by the intestine partitions and into the bloodstream, these molecules can journey to the mind. The micro organism additionally work together with immune cells. This may not directly have an effect on the mind by way of immune cell signaling pathways, or, in late neurodegenerative illness levels, straight have an effect on the mind. During the late illness levels, it’s potential that immune cells infiltrate the mind from the bloodstream, by way of extra porous blood vessels.
The function of intestine micro organism in neurodegenerative illnesses remains to be an rising discipline of analysis. “There’s some rightful skepticism,” stated Timothy Sampson, assistant professor of physiology at Emory University.
“It is still a relatively young field, so there are a lot of unknowns,” stated Jan Pieter-Konsman, a neuroimmunologist on the University of Bordeaux. Until not too long ago, research of the intestine microbiome and neurodegenerative illnesses had been restricted to evaluating microbial communities in folks with and with out the illnesses. Most research didn’t look deeper on the operations inside these ecosystems.
“You’ve got to break down that community to understand those interactions,” stated Maureen O’Malley, a philosophy of microbiology researcher on the University of Sydney. But prior to now 5 years, teams are more and more drilling into these interactions, learning which particular microbes and molecules could possibly be concerned in illness.
Parkinson’s illness, particularly, has captured the eye of researchers within the gut-brain axis. Gastrointestinal points, like constipation, typically happen in folks years earlier than they develop the movement-related signs attribute of the illness.
“One of the cardinal features originally of James Parkinson’s diagnosis of ‘the shaking palsy,’ which has become Parkinson’s disease, was this observation of intractable constipation in patients,” stated Lynne Barker, affiliate professor of cognitive neuroscience at Sheffield Hallam University. The incontrovertible fact that the intestine is concerned in Parkinson’s hasn’t been a secret.
Scientists take a look at bacterial genes in stool samples to approximate the bacterial composition of the intestine. These research have proven that microbiomes of individuals with Parkinson’s differ from these with out Parkinson’s. These variations come up independently of different influences over the microbiome, like weight-reduction plan. “But that leads to this big chicken-and-the-egg problem,” stated Sampson. “Did the disease cause the microbiome to change, or did the change in the microbiome influence the disease?”
In a small, preliminary examine, Purna Kashyap, professor of drugs and physiology and co-director of the microbiome program at Mayo Clinic, and his crew used mouse fashions of Parkinson’s illness and confirmed that mice needed gut bacteria to develop movement-related symptoms. In germ-free mice, ones with none detectable micro organism, fungi or viruses in or on their our bodies, motion issues by no means materialized.
Studies in rats and mice have additionally proven that the intestine micro organism Escherichia coli make proteins akin to alpha-synuclein protein clumps that kind within the mind in Parkinson’s illness. In mice engineered to overexpress alpha-synuclein, Sampson has shown that this bacterial protein within the intestine exacerbates each alpha-synuclein aggregation within the mind and motion signs.
O’Malley cautioned that whereas these animal experiments go deeper than earlier research, they need to be interpreted with warning, since animal research typically fail to duplicate in people. But, she stated, “I think you can still get some of the suggestive findings that then allow you to build a better model of what’s going on.”
More not too long ago, just a few analysis teams have began in search of intestine microbiome disturbances in different neurodegenerative illnesses, like Alzheimer’s. Protein clumps known as beta-amyloid plaques disrupt mind cell capabilities in folks with Alzheimer’s. Mouse fashions of Alzheimer’s illness additionally recommend a task for intestine microbes.
“If you keep those mice germ-free, they don’t develop as many amyloid plaques,” stated Barbara Bendlin, a professor of drugs on the University of Wisconsin, Madison. “It does really suggest that in some way there’s a link between microbes and the development of Alzheimer’s disease pathology.”
As a place to begin in human analysis, Bendlin and her crew have studied gut microbiomes of people with Alzheimer’s disease by analyzing stool samples. In a small examine of 25 folks with Alzheimer’s and 25 folks with out, they discovered that Alzheimer’s sufferers had a much less numerous bacterial inhabitants and totally different quantities of sure micro organism. They additionally analyzed the cerebrospinal fluid, which surrounds the mind and spinal twine, of members to search for relationships between Alzheimer’s-related biomarkers and the intestine microbiome.
“We found that there were relationships between the gut microbiome and those cerebrospinal fluid biomarkers, even among individuals who were asymptomatic,” stated Bendlin. “That suggested to us that maybe there’s a link between the gut and brain pathology that’s present even before people develop dementia.”
Scientists have additionally begun exploring hyperlinks between intestine micro organism and ALS, a illness wherein neurons powering the muscle mass progressively die. In a examine of mice with a genetic mutation identified to trigger ALS in some human instances, Eran Blacher, postdoctoral fellow learning the gut-brain axis on the neurology division of Stanford University School of Medicine, and his crew confirmed that gut microbiome changes preceded ALS symptoms. Blacher stated that indicated that such adjustments might need to do with the illness.
The researchers additionally discovered that sure intestine micro organism produced molecules that altered the illness in mice. Giving the mice a probiotic complement with that micro organism boosted ranges of the molecule nicotinamide and improved their signs. Nicotinamide produces key chemical compounds for mobile pathways scientists suppose are concerned in ALS. “So we can change the disease progression and manifestation by treating the mice with specific bacteria, which was very surprising,” stated Blacher.
Blacher’s preliminary findings in a small group of human sufferers supported these outcomes: People with ALS had decrease ranges of bacterial genes wanted for nicotinamide metabolism of their stool samples in comparison with folks with out ALS. They additionally had decrease ranges of nicotinamide of their blood and cerebrospinal fluid. “We are not saying that we were able to cure ALS, or to change anything in disease progression in humans,” stated Blacher. Rather, bigger follow-up research may reveal extra about mechanisms underlying ALS and reveal potential remedy targets.
But general, the microbiome’s function in neurodegenerative illnesses stays mysterious. Barker’s group is analyzing knowledge from a small feasibility examine to see whether or not administering a standard probiotic to folks with Parkinson’s illness may change their microbiome composition or affect high quality of life. Unlike earlier work, Barker stated her group is wanting past big-picture adjustments in microbial communities to zero in on particular bacterial species.
Still, research are removed from revealing microbiome-based therapies for neurodegenerative illnesses. Even if some type of probiotics or dietary adjustments had been proven to be efficient at assuaging some signs, it wouldn’t be a remedy for these difficult illnesses. If intestine microbes are concerned in neurodegeneration, scientists additionally want to determine how this matches with different potential illness causes.
“We have not learned the mechanisms that link that to the brain, and until we firmly know those, we’re not going to be able to develop effective treatments,” stated Bendlin.
Jackie Rocheleau is a contract journalist and editor primarily based in upstate New York. She writes about neuroscience, public well being, and drugs. Follow her on Twitter at @JackieRocheleau.
#Ecosystems #Guts #Linked #Brain #Disorders
https://gizmodo.com/how-the-ecosystems-in-our-guts-could-be-linked-to-brain-1847573290